Eyelid skin is the thinnest on the body and as such is particularly vulnerable to damage from ultraviolet light.
This in turn increases the chance of skin cancers developing. There are many different types of skin cancer but 3 together are the commonest: Basal cell carcinoma; Squamous cell carcinoma; Melanoma.
 Top left: Basal Cell Carcinoma of the lower eyelid with loss of eyelashes; Top right: Excision of Basal Cell Carcinoma; Bottom left: Hughes Flap reconstruction with skin graft; Bottom right: Reconstruction of lower eyelid completed
Top left: Basal Cell Carcinoma of the lower eyelid with loss of eyelashes; Top right: Excision of Basal Cell Carcinoma; Bottom left: Hughes Flap reconstruction with skin graft; Bottom right: Reconstruction of lower eyelid completed
What is Basal Cell Carcinoma?
Basal cell carcinoma (also known as a rodent ulcer) is a malignant growth of the skin. Unlike many other types of cancer it tends not to spread to the rest of the body. It has the best prognosis of all of the skin cancers, as long as it is completely removed. It usually presents as a slow growing lump on the skin. This lump may have an ulcer or non healing centre. It may be itchy or recurrently bleed. If it is in the line of eyelashes, these lashes may be lost.
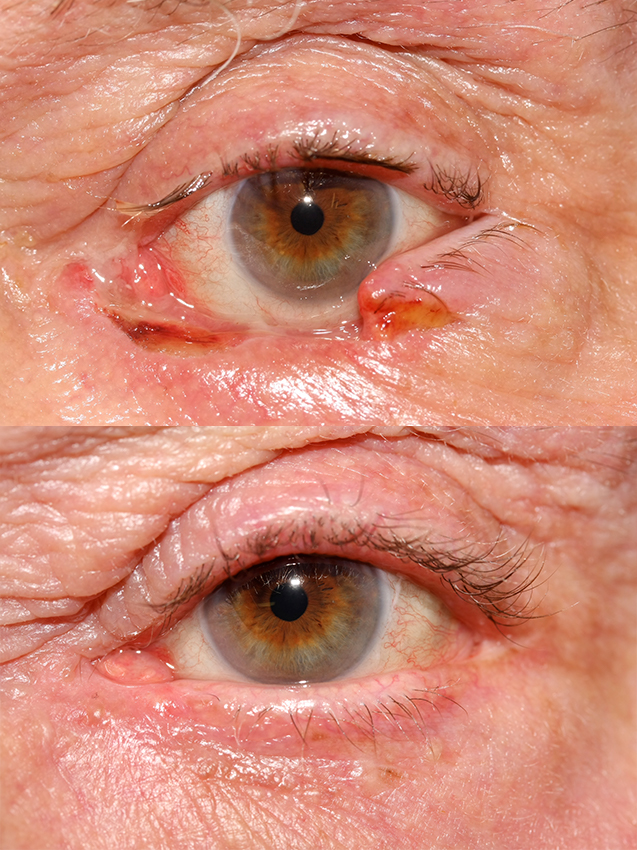
 Top - Basal Cell Carcinoma between the eyelid and the nose; 2nd image - After excison with dressing still in place; 3rd image - reconstruction with a local skin flap; Bottom - final result
Top - Basal Cell Carcinoma between the eyelid and the nose; 2nd image - After excison with dressing still in place; 3rd image - reconstruction with a local skin flap; Bottom - final result
What is Squamous Cell Carcinoma?
Squamous cell carcinoma is a malignant growth of the skin. There is a spectrum of disease with milder forms confined to the visible lump and more severe types that have the potential to spread to the rest of the body. If it is completely removed it has a good prognosis. It usually presents as a lump or ulcer on the skin. It may be itchy or recurrently bleed. If it is in the line of eyelashes, these lashes may be lost. It may have a prominent crust or scale associated with it.

Top - right lower eyelid basal cell carcinoma; 2nd image - left arrow is a benign naevus, right arrow is the BCC; 3rd image - after reconstruction with local sliding skin flap; Bottom - final result
What is Melanoma?
A melanoma is a malignant cancer of melanocyte cells in the skin. Melanocytes are the cells in the skin that carry the pigment melanin and give skin its brown colour. Most melanomas are brown but some are amelanotic or flesh coloured. It is a rare cancer. Wide excisions are necessary and if caught early enough this may be curative. Unfortunately in some cases the tumour has already spread (metastatic) by the time it is removed. If so it may be treatable with chemotherapy. It usually presents as a small brown lump in the skin. There may be different shades of brown and the border may be irregular. It will get bigger with time. It may itch or bleed. If you have a new area of brown skin or an old one that has changed you should see your general practitioner or a dermatologist
What is eyelid skin cancer excision and reconstruction surgery?
These are operations to completely remove skin cancer and then to reconstruct / rebuild the defect left after the excision. The aim of excision is to remove all of the cancer. The aim of the reconstruction is to provide a good functional outcome e.g. an eyelid that can protect the surface of the eye and a good cosmetic outcome.
Top - after excision of right lower lid basal cell carcinoma; Bottom - after reconstruction by lateral release and direct closure
What are the benefits of surgery?
Surgical excision of skin cancer gives the best chance that a tumor will not come back. It allows examination of the specimen by a pathologist in the laboratory under a microscope. This enables us to determine if we have removed all of the cancer.

Top - basal cell carcinoma between the eyelid and the nose; Middle - after excision; Bottom - after reconstruction by direct closure
Excision of skin cancer
What is Excision with Direct Closure?
For small tumours it may be possible to excise and reconstruct at one operation, by simply stitching the two edges of the wound together. This is excision with direct closure. If the pathology report 1 week after this shows that the tumour has not been completely removed it is possible to go back to theatre and remove further tissue at a later date. If the defect is too big to close directly and requires a skin flap or graft, the reconstruction must wait until the pathology report is received. This is known as excision with delayed reconstruction.
What is Excision with Delayed Reconstruction?
The skin cancer is removed in theatre and a dressing is applied and secured with surgical tape. You will go home the same day and the dressing stays in place for a week. 1 week later you will come back to theatre and have the surgery to reconstruct the defect. During the week between operations the pathologist will be able to examine the excised tumour and tell if it has been completely removed. We need this ‘all clear’ pathology report before we can carry out the reconstruction. If it is not ‘all clear’ further excision will be necessary and the reconstruction may be delayed a further week. It is uncommon for the first excision to be incomplete and most people have their reconstruction 1 week later.
What is Excision with Frozen Section Control?
In some cases a tumour may be excised at the beginning of the operating list and reconstructed at the end of the same operating list. The excised tumour is sent urgently to the pathologist who freezes it and examines it immediately. He then tells the surgeon if he can reconstruct or excise further. This method is usually reserved for tumours where multiple excisions may be necessary.
What is Mohs Excision Surgery?
Mohs surgery is carried out by a dermatologist who has been specially trained in this technique. This is usually at a clinic in another hospital. The skin cancer is removed in thin slices. Each slice is looked at immediately by the Mohs surgeon. The Mohs surgeon keeps excising until he is certain all of the tumour is removed. This is most suitable for squamous cell carcinoma and basal cell carcinoma, particularly when the margin of the tumour is difficult to see with the naked eye or when tumour is recurrent after previous reconstruction. The reconstruction takes place usually within 2 days
Recontruction
When a skin cancer is removed it leaves a defect or ‘hole’ in the skin. Reconstruction is surgery to repair this defect. There are many different reparative techniques. Each person and each defect are different and your consultant will discuss the appropriate techniques and options with you. Some reconstructions involve some or all of the techniques described below
What is Direct Closure?
Direct closure of a wound is simply bringing the two edges of a wound together with buried, deep, absorbable sutures and skin sutures which may be absorbable or non-absorbable. It is appropriate in smaller defects where there is enough skin laxity to allow closure of the wound.
What is a skin graft?
A full thickness skin graft involves the transfer of a piece of skin from a donor site where there is relative excess of skin, to the defect (excision site) also known as the host site. The donor site is closed directly. The skin graft is sutured into place with either absorbable or non-absorbable sutures. There are various donor sites (where skin can be taken from for use in reconstruction) commonly used for reconstruction around the eyes. They include: upper eyelid; infront of the ear; behind the ear; behind the collar bone; upper inner arm.
What is a skin flap?
A skin flap is similar to a skin graft except that the donor skin is not completely detached. This means that it retains some of its own blood supply which usually produces superior results. A skin flap donor site is usually immediately adjacent to the defect, allowing the skin flap to be mobilised and rotated or slid into place in the defect.
What is a Hughes flap?
For large reconstructions of the lower lid it may be necessary to use a Hughes flap reconstruction. Part of the inside of the upper eyelid is mobilised and pulled down over the eye like a ‘roller blind’ into the defect in the lower eyelid. This is the Hughes flap. A skin graft is then placed on top of the Hughes flap. The tissue covering the eye will stay in place for 4 weeks. During this time you will not be able to see out of the eye because it will be covered by the Hughes flap. 4 weeks after the reconstruction a short second stage operation will be carried out in theatre to divide the tissue coming down from the upper eyelid. The eyelids will immediately open and vision will return.
What are the alternatives to surgery for eyelid skin cancer?
Alternatives to surgery depend on the type of skin cancer. Basal cell carcinomas are suitable in some cases to non-surgical treatments however others such as melanoma are not. Your consultant will discuss this with you.
Radiotherapy. Small basal cell carcinomas on the eyelid margin may be well treated by this method. It is also used for larger lesions when the risks of surgery are too great for that individual, when a person declines surgery or when total excision is not possible.
Cryotherapy. Small basal cell carcinomas that have not invaded deeply may be treated with cryotherapy. This is particularly suitable for people who are not fit for surgery or those who have conditions that predispose them to multiple skin cancers. It is applied using a cryoprobe that looks like a pen with a cold tip or with a liquid nitrogen spray.
What will happen if I decide not to have surgery?
Skin cancer does not spontaneously get better. Over time it will gradually grow. It will start to destroy normal tissue, grow deeply and may ulcerate and bleed. Eventually eyelid skin cancer may grow into the orbit. In this situation the only surgical option for curative excision is an exenteration or complete removal of the eyelids, eye and orbital tissue. Basal cell carcinoma does not normally spread to the rest of the body. It grows and invades tissue directly. Squamous cell carcinoma and Melanoma can spread to the rest of the body. Declining surgery for any of these or other types of skin cancer may result more extensive surgery at a later date or even allow the spread of the cancer to other parts of the body. Surgical removal of these lesions does not prevent distant spread (this may have already occurred at the time of surgery) but it is your best chance of reducing the risk of it happening.
What will happen before surgery?
Before the operation you will be seen in the clinic by Mr McCormick. You may also be seen by another doctor who is a member of the team. Mr McCormick will ask you about your problem. He/she will also ask about other medical problems you have medications you take and any allergies (bring a list or the tablets themselves with you). Mr McCormick will examine your eyes and will determine if you are suitable for surgery. He will explain exactly what type of surgery he will be carrying out. If you are to proceed with surgery the operation will be discussed in detail. This will include any risks or possible complications of the operation and the method of anaesthesia. You will be asked to read and sign a consent form after having the opportunity to ask any questions. You will also see a preoperative assessment nurse. He/she will carry out blood tests and an ECG (heart tracing) if required. He/she will also advise you if you need to starve before the operation.
What should I do about my medication?
Mr McCormick will want to know all the medication that you take and about any allergies you have. In some cases you may be asked to stop or reduce the dose of blood thinning tablets like: warfarin, apixaban, dabigatran, aspirin, clopidogrel (plavix), dipyridamole (persantin). This decision is made on an individual basis and you should only do so if it is safe and you have been instructed by your GP, surgeon or anaesthetist. This will be discussed with you before surgery. Other medication should be taken as usual. You should avoid herbal remedies for 2 weeks prior to surgery as some of these may cause increased bleeding at the time of surgery.
What are the risks and possible complications of surgery?
All surgery caries a risk of bleeding and infection, both are fortunately uncommon in these operations.
Infection might present as increased swelling and redness of the skin. There might also be yellow discharge from the wound. It is treated with antibiotics.
Bleeding may appear as blood staining of the eye pad applied after surgery or blood running down your cheek. This is different to slightly blood stained tears which is normal after surgery.
Usually sitting upright and applying a cool compress to the area will stop minor bleeding. If this does not stop the bleeding you should call your GP, contact the ward on which you were admitted or visit an accident and emergency department.
Whenever the skin is incised a scar may form. Every attempt is made by the surgeon to minimise and hide scars but sometimes they can be visible.
The site of surgery is in close proximity to the eyeball. Although extremely unlikely, whenever surgery is carried out close to the eye there is a potential risk of damage to the eye and therefore to eyesight.
What type of anaesthetic can I have for the surgery?
You should have the opportunity to discuss the risks and benefits of different anaesthesia with your surgeon or anaesthetist prior to surgery.
Three types of anaesthesia are used for these procedures: local anaesthetic alone; local anaesthetic with intravenous sedation and general anaesthesia.
Local anaesthetic alone means an injection of local anaesthetic into the skin where the surgery will take place. It is similar to having dental injections. The initial injection is painful but usually within 30 seconds the injection is complete.
Sedation means that you are awake, breathing for yourself and don’t have a breathing tube inserted but you are very relaxed and sleepy and often don’t remember the operation.
General anaesthetic means you are completely asleep with a breathing tube inserted.
What should I expect after surgery?
After surgery you may experience some pain. Simple paracetamol is usually enough to control this. The eyelids may be bruised and swollen, which may take up to 2 weeks to settle.
Post operative Instructions
After Excision – awaiting reconstruction 1 week later
Pad to remain in place until returning for reconstructive surgery
If the pad becomes loose, chloramphenicol should be applied to the wound and eye four times a day.
After Reconstruction
Pad for 24 hours.
Apply chloramphenicol ointment to the skin wound 3 times a day for 2 weeks
Clinic review 1 week when any non-dissolvable sutures may be removed
Clean any incisions with boiled water that has cooled down and simple cotton pads

